
October 2, 2024
Nerve blocks have long been a cornerstone in the treatment of chronic pain, providing relief for patients where other interventions fall short.
However, this seemingly simple technique has rapidly evolved, with new research and innovative technologies pushing the boundaries of what is possible in modern pain management.
This blog delves deeper into the science, mechanisms, latest advancements, and future applications of nerve blocks in both clinical and therapeutic settings.
Let’s see the topics for our blog!
At their core, nerve blocks work by interrupting the transmission of pain signals from specific nerves to the brain.
This interruption is achieved by injecting a local anesthetic (often combined with steroids or other agents) near a nerve or nerve cluster. But how does this process work at a cellular and neurological level?
Understanding Nerve Blocks: The Mechanism of Action
- Ion Channel Modulation: Local anesthetics work primarily by inhibiting sodium channels in the nerve cells, which prevents depolarization and the propagation of pain signals.
- Inflammatory Pathway Suppression: When corticosteroids are included in the injection, they play a role in reducing inflammation by downregulating pro-inflammatory cytokines and other mediators that contribute to persistent pain.
- Peripheral vs. Central Effects: While the direct target of nerve blocks is often a peripheral nerve, the effects on central nervous system sensitization and plasticity are profound.

Types of Nerve Blocks and Their Expanding Applications
In practice, nerve blocks are highly versatile. They can be tailored to address various pain conditions, depending on the nerves involved.
Below are some of the most commonly used blocks, along with their expanding use in clinical scenarios:
- Epidural Blocks: Traditionally used in labor pain and spinal conditions, recent advances have explored their use in treating radicular pain associated with disc herniation and spinal stenosis.
- Sympathetic Nerve Blocks: Often used in conditions like complex regional pain syndrome (CRPS) or vascular pain, research is now investigating their effectiveness in managing autonomic dysfunctions such as hyperhidrosis or Raynaud’s disease.
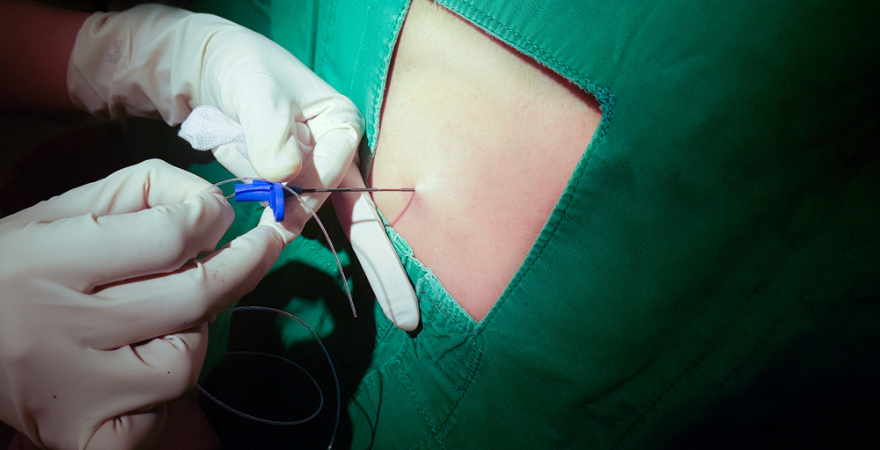
- Peripheral Nerve Block: Commonly employed for postoperative pain management, recent innovations include the use of continuous catheter-based nerve blocks that allow for prolonged pain relief without the need for opioids, offering a potential solution to the opioid crisis.
- Stellate Ganglion Blocks: Traditionally indicated for facial or upper extremity pain, newer research is uncovering its potential role in treating PTSD and mood disorders by targeting the autonomic nervous system’s role in emotional regulation.
Innovations in Nerve Block Technology
As medicine moves toward precision and minimally invasive approaches, the nerve block procedure is also benefiting from groundbreaking technological advancements.
- Ultrasound-Guided Precision: The introduction of ultrasound-guided nerve blocks has transformed the accuracy of the procedure. It allows clinicians to visualize nerves and surrounding tissues in real-time, leading to more precise injections, reducing risks of complications, and improving patient outcomes.
- Neurolytic Agents for Chronic Conditions: In cases of severe chronic pain, chemical neurolysis using agents like phenol or alcohol can provide long-term relief by permanently damaging the nerve.
- Cryoablation and Radiofrequency Nerve Blocks: These techniques go beyond temporary relief, offering long-lasting pain management by freezing or thermally ablating the nerve fibers responsible for pain transmission.
Nerve Blocks in the Age of Personalized Medicine
The future of nerve blocks lies in personalization. By integrating genetic and biomarker analyses into pain management protocols, clinicians are increasingly able to predict which patients will respond best to nerve block interventions.
- Genetic Predictors of Pain Sensitivity: Ongoing studies are examining how genetic variations in pain receptors (like the sodium channel gene SCN9A) can influence the effectiveness of nerve blocks, paving the way for tailored treatment plans.
- Biomarkers for Chronic Pain: Researchers are also looking at specific biomarkers (e.g., neuroinflammation indicators) that can help predict the likelihood of chronic pain becoming resistant to standard treatments.

Addressing Common Misconceptions
While nerve blocks are effective, several myths continue to circulate in both patient and provider communities. These misconceptions need addressing to ensure the procedure is used optimally:
- Nerve blocks are only for temporary relief: While some nerve blocks provide short-term pain relief, others, like neurolytic blocks or ablations, offer long-lasting solutions. The treatment plan is always tailored to the patient’s unique needs.
- Nerve blocks mask the pain, but don’t treat the cause: In many cases, such as inflammatory conditions, nerve blocks can significantly reduce the underlying pathology by lowering inflammation and breaking the cycle of chronic pain.
- Nerve blocks are invasive and risky: With modern techniques like ultrasound guidance, the risks of complications are minimal.
The Future of Nerve Blocks: Where Do We Go From Here?
The evolution of nerve blocks is not slowing down. With ongoing research into advanced imaging, personalized medicine, and novel neurolytic agents, the possibilities for treating pain are expanding rapidly.
In conclusion, nerve blocks represent much more than a simple pain relief technique. They are a dynamic and evolving tool that, when combined with emerging technologies, may redefine the landscape of pain management in the coming decades.


